The SPADE tool has been designed to assist medical professionals define the probability of axial spondyloarthritis in a patient with chronic back pain, below the age of 45 with no definitive changes on X-ray
In your patient with chronic back pain, tick all the symptoms that apply to determine the likelihood of axial spondyloarthritis
ASAS have outlined the criteria for identifying inflammatory back pain. It is useful to phrase the questions to your patients in the following way:
- Inflammatory back pain usually begins in the third decade of life and is unlikely to have an onset after 45 years
- It is important to ascertain the patient's age at the onset of the back pain and as opposed to only recording their current age as they may have been experiencing back pain for several years
- Unlike inflammatory back pain, mechanical back pain, such as herniation, is frequently of a more sudden onset. IBP has an insidious onset and patients are likely to have been experiencing back pain for > 3 months.
- Symptoms of musculoskeletal inflammation are often improved with movement and exercise.
- Similar to the above, no improvement of the pain with rest is a classic feature of inflammatory back pain.
- Patients with inflammatory back pain often experience a worsening of symptoms when resting at night, and waking during the second half of the night due to pain and discomfort is a key feature of inflammatory back pain.
Inflammatory back pain requiring further investigation is usually indicated if the answer is ‘yes’ to 4 or more of these parameters.
In addition to these key distinguishing features, as outlined by the ASAS criteria for inflammatory back pain, other signs of inflammatory back pain to look out for include:
- Good response to NSAIDs
- Alternating buttock pain
- Waking during the second half of the night
- Morning stiffness : pain and stiffness for > 30 minutes after rising in the morning
3. Rudwaleit, M et al. Arthritis Rheum 2005 ;52:1000-8. 4. Marzo-Ortega, H et al. Ann Rheum Dis 2009 ;68:1721-2.
This figure was developed by, and is the intellectual property of, the UK Axial SpA Special Interest Group: Dr Nick Barkham, Dr Alex Bennett, Dr Karl Gaffney, Dr Amanda Isdale, Dr Andrew Keat, Dr Helena Marzo-Ortega, Dr Raj Sengupta
This website is intended for healthcare professionals (GPs, physiotherapists, osteopaths, chiropractors, nurses and rheumatologists) who see patients <45 years with chronic back pain (>12 weeks). The website is not designed for use by patients with back pain.
- 'Axial SpA improbable' – your patient is unlikely to have Axial Spondyloarthritis. Consider other potential diagnoses to explain the patients chronic back pain.
- 'Additional tests necessary' – consider further tests such as HLAB27 testing or MRI
- 'Probable diagnosis of Axial SpA' – your patient is likely to have Axial Spondyloarthritis. Ensure that other possible diagnoses have been excluded.
- 'Definitive diagnosis of Axial SpA' – it is very likely that your patient has Axial Spondyloarthritis
This website is not designed to replace the clinician who has trained for many years to diagnose patients. It is designed to be a decision aid for those who do not commonly see patients with inflammatory spinal disease.
Any patients who are in the 'additional tests necessary, probable or definitive diagnosis of Axial SpA' should be referred to a rheumatologist. If the clinician is comfortable with organising appropriate additional tests, this can be done for those patients in the 'additional tests necessary' category. The patients in the 'Axial SpA improbable' category should be re-evaluated for an alternative diagnosis.
This website provides a clinical tool based on published research. It is not meant to be a substitute for a clinician with expertise in Axial Spondyloarthritis. This website cannot be held responsible for missed diagnoses of Axial Spondyloarthritis nor any other conditions which may explain the patients back pain.
- Rudwaleit M, van der Heijde D, Khan MA, Braun J, Sieper J. How to diagnose axial spondyloarthritis early. Ann Rheum Dis. 2004 May;63(5):535-43.
- Feldtkeller E(1), Rudwaleit M, Zeidler H. Easy probability estimation of the diagnosis of early axial spondyloarthritis by summing up scores. Rheumatology (Oxford). 2013 Sep;52(9):1648-50.
- Zeidler H, Mau R, Mau W et al. Evaluation of early diagnostic criteria including HLA-B27 for ankylosing spondylitis in a follow-up study. Z Rheumatol 1985;44: 249-53.
- Mau W, Zeidler H, Mau R et al. Outcome of possible ankylosing spondylitis. Clin Rheumatol 1987;6(Suppl 2): 60-6.
- Mau W, Zeidler H, Majewski A et al. Evaluation of early diagnostic criteria for ankylosing spondylitis in a 10 year followup. Z Rheumatol 1990;49:82-7.
- Amor B, Dougados M, Mijiyawa M. Critères de classification des spondylarthropathies. Rev Rhum 1990;57: 85-9.
- Amor B, Dougados M, Listrat V et al. Èvaluation des critères des spondylarthropathies d'Amor et de l'European Spondylarthropathy Study Group (ESSG). Ann Mèd Interne 1991;142:85-9.
- Rudwaleit M, van der Heijde D, Khan MA et al. How to diagnose axial spondyloarthritis early? Ann Rheum Dis 2004;61:535-43.
- Rudwaleit M, Feldtkeller E, Sieper J. Easy assessment of axial spondyloarthritis (early ankylosing spondylitis) at the bedside. Ann Rheum Dis 2006;65:1251-2.
- Grimes DA, Schulz KF. Refining clinical diagnoses with likelihood ratios. Lancet 2005;365:1500-5.
- Calin A, Porta J, Fries JF et al. Clinical history as a screening test for ankylosing spondylitis. JAMA 1977;237: 2613-4.
- Rudwaleit M, Metter A, Listing J et al. Inflammatory back pain in ankylosing spondylitis—a reassessment of the clinical history for classification and diagnosis. Arthritis Rheum 2006;54:569-78.
- Weber U, Lambert RG, Østergaard M et al. The diagnostic utility of magnetic resonance imaging in spondylarthritis: an international multicenter evaluation of one hundred eighty-seven subjects. Arthritis Rheum 2010;62: 3048-58.
- Weber U, Østergaard M, Lambert RG et al. The impact of MRI on the clinical management of inflammatory arthritides. Skeletal Radiol 2011;40:1153-73.
- Sieper, J et al. New criteria for inflammatory back pain in patients with chronic back pain: a real patient exercise by experts from the Assessment of SpondyloArthritis international Society. Ann Rheum Dis 2009; 68:784-788
- Rudwaleit, M et al. Inflammatory back pain in ankylosing spondylitis: a reassessment of the clinical history for application as classification and diagnostic criteria. Arthritis Rheum 2006; 54:569-578
- Braun A, Saracbasi E, Grifka J, Schnitker J, Braun J. Identifying patients with axial spondyloarthritis in primary care: how useful are items indicative of inflammatory back pain? Ann Rheum Dis. 2011 Oct;70(10):1782-7.
- van den Berg R, de Hooge M, Rudwaleit M, Sieper J, van Gaalen F, Reijnierse M, Landewé R, Huizinga T, van der Heijde D. ASAS modification of the Berlin algorithm for diagnosing axial spondyloarthritis: results from the SPondyloArthritis Caught Early (SPACE)-cohort and from the Assessment of SpondyloArthritis international Society (ASAS)-cohort. Ann Rheum Dis. 2013 Oct;72(10):1646-53.
- Hermann J, Giessauf H, Schaffler G, Ofner P, Graninger W. Early spondyloarthritis: usefulness of clinical screening. Rheumatology (Oxford). 2009 Jul;48(7):812-6.
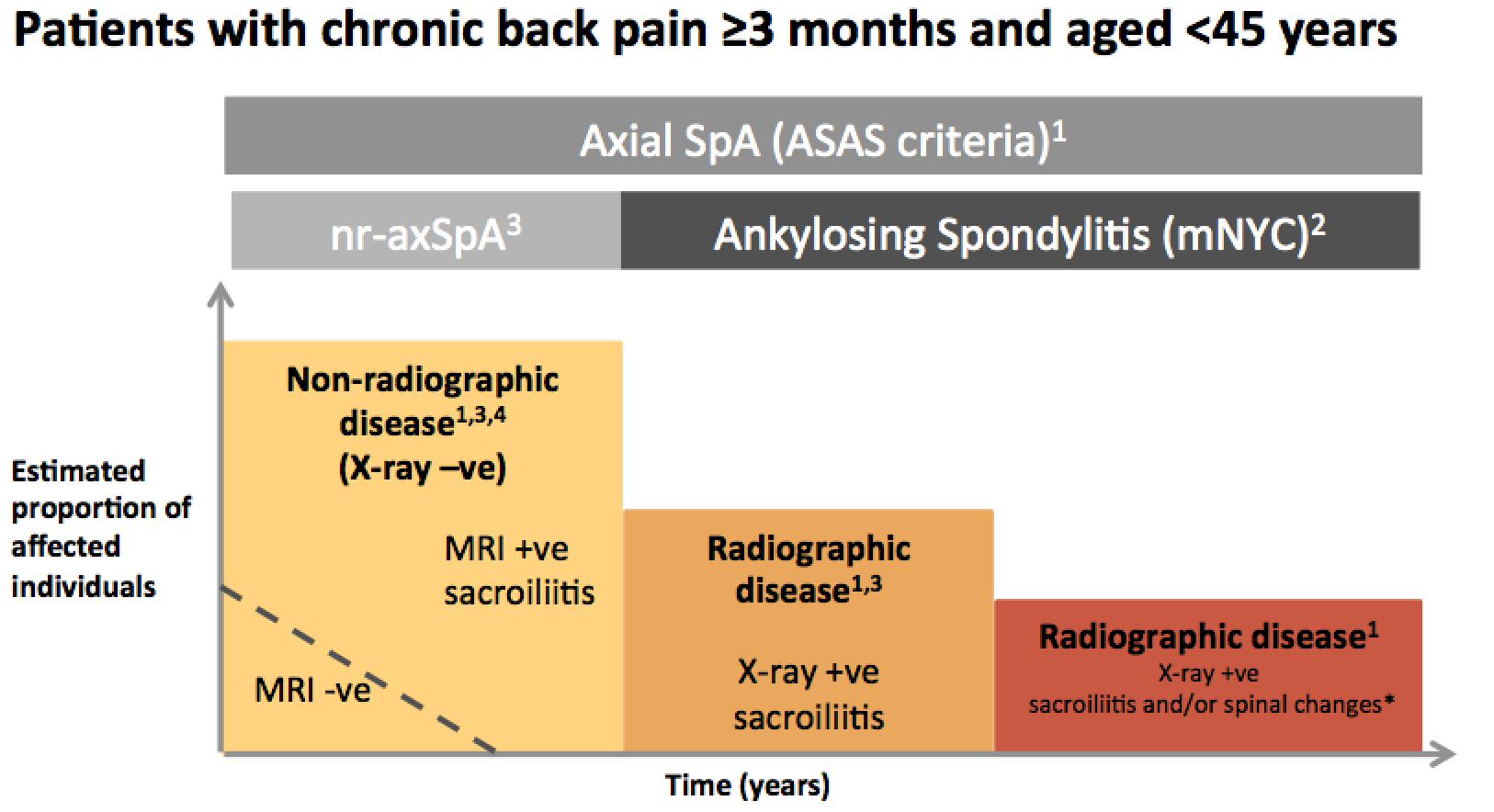
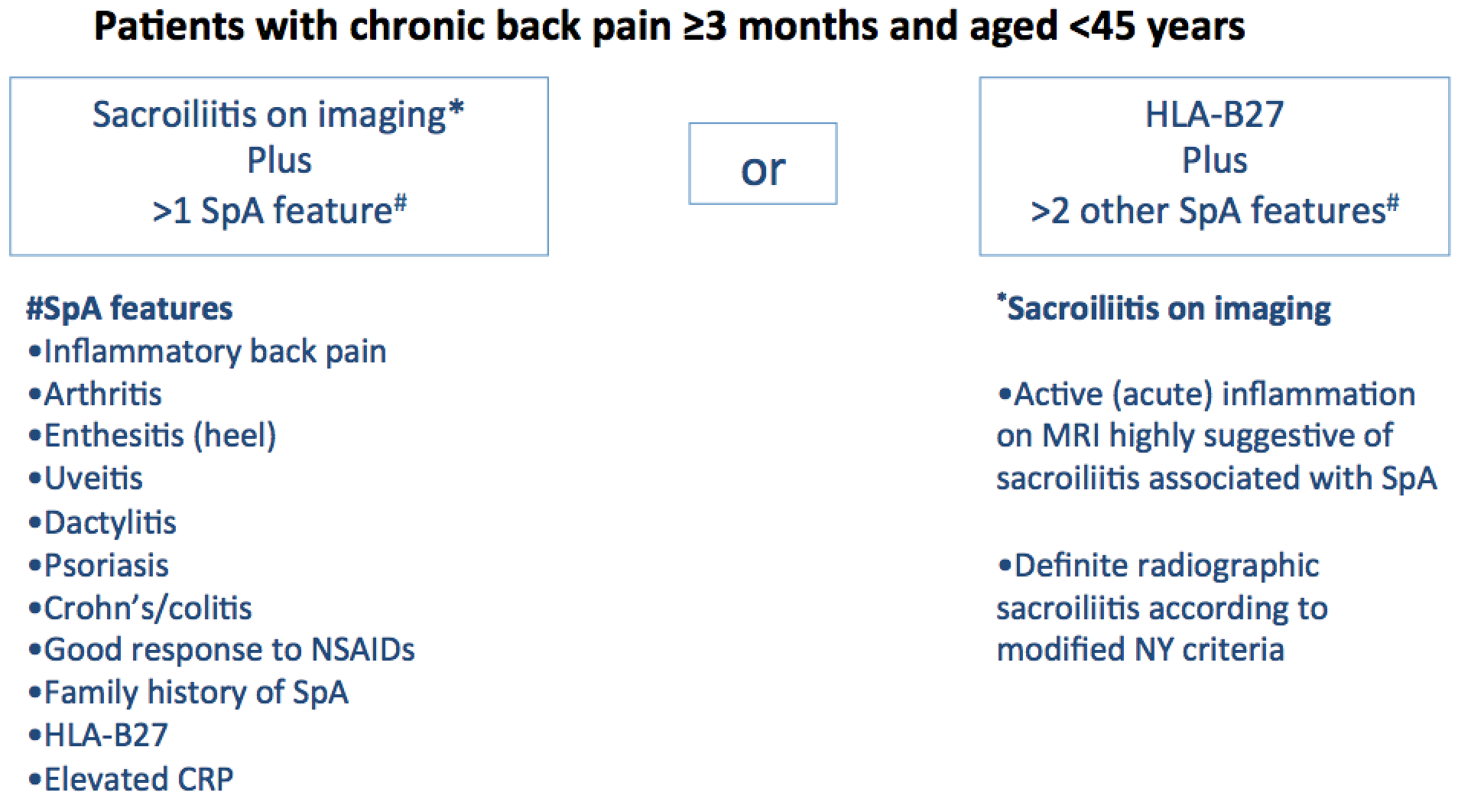
The SPADE tool has been developed to reduce the delay in diagnosis of patients with Axial Spondyloarthritis (AxSpA). Several validated criteria sets exist to aid the diagnosis of AxSpA.
Many referral strategies have been devised to optimize the diagnosis of AxSpA. Studies have shown that these strategies result in the diagnosis of AxSpA in 30 to 40% of patients referred to secondary care.
There are 2 issues with these referral strategies. Whilst these strategies are simple, they require clinicians to remember the specific criteria sets and apply them in busy clinical settings. Furthermore, with financial constraints in healthcare, ensuring that only the patients that need to be assessed in secondary care are referred is paramount. As a result strategies to improve the diagnosis of AxSpA in secondary care to over 40% should be explored.
The ease of access of tools such as SPADE is critical to ensure that clinicians will use it to aid decision making. An similar example of a web based tool is the FRAX tool, which aids decision making in patients with osteoporosis.
A quantitative estimation of the probability of axial SpA in a young patient with chronic back pain has been previously proposed. This approach involves multiplying the likelihood ratios of SpA specific features. The simplification of this approach was suggested by Feldtkeller et al in 2013. The SPADE tool has been developed based on the Feldtkeller adaptation. The probability of Axial SpA derived from the 'SPADE Tool' is displayed on a chart with clear instructions for the user on what action should be taken next.
This tool is not intended to replace the clinician assessing a person with possible ankylosing spondylitis. One of the key reasons being that the tool does not incorporate any negative findings in the diagnostic algorithm. The clinicians diagnostic skills, which include the ruling out of other possible diagnoses, remains of significant importance.